Diabetic retinopathy
In addition to causing cataract, diabetes can lead to diabetic retinopathy. In this section, we take a closer look at what is meant by the term diabetic retinopathy as well as the treatments available.
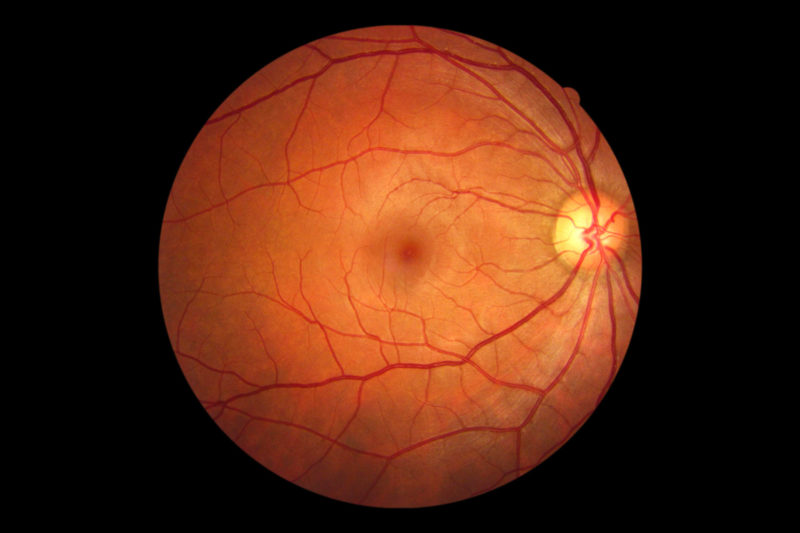
The retina is the light sensitive tissue in the back of the eye. It is the ‘brain’ of the eye where light is converted into electrical signals transferred through the optic nerve to the brain which converts them into the images that we perceive. A healthy retina is essential for good vision.
Diabetic Retinopathy (DR) refers to the damage that can occur in the retina in patients with diabetes; it usually takes a number of years for these changes to develop. They affect the small retinal vessels and if left untreated they lead to severe loss of vision or even blindness.
The walls of these defective vessels become fragile and initially leak fluid and blood around them. Eventually they may become blocked off so that oxygen and other nutrients are not transferred properly to the photosensitive cells of the retina. It is then that patients experience problems with their vision where black spots may appear.
DR is actually is a major cause of poor vision in the UK. It is estimated that in England every year 4,200 people are at risk of blindness caused by diabetic retinopathy and there are 1,280 new cases of blindness caused by diabetic retinopathy.
STAGES / CLASSIFICATION OF DIABETIC RETINOPATHY
DR can be classified into different stages according to which part of the retina is affected and how severe the damage is. The most important stages are:
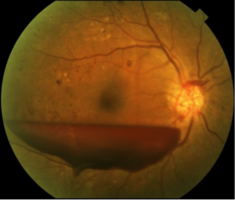
Background Diabetic Retinopathy (BDR): In BDR, initial changes in the retina are observed. These include:
- tiny haemorrhages which come from retinal vessels,
- yellow-waxy deposits in the retina that correspond to lipids leaking through defective vessels

Proliferative Diabetic Retinopathy: In PDR, the oxygen supply to the retina is not enough. As a result retinal cells actually starve and die. When this occurs, the body is trying to make new vessels in their place (a process called NeoVascularization). These new vessels can be located on the optic nerve/disc or elsewhere in the retina. They are fragile and can easily bleed into the eye or they can transform into scarring tissue causing profound vision loss. PDR if left untreated will lead into blindness.

Advanced Diabetic Eye Disease: This is the stage following PDR. The scarring caused by PDR may be so severe that the retina can be detached from the back of the eye. Persistent haemorrhaging continues, the eye also can develop high pressures and become painful.
Maculopathy : This term refers to damage affecting the macula which is the part responsible for clear-detailed vision. If it is affected then patients usually experience blurring of vision. Reading or recognizing faces become problematic. Fluid can accumulate causing cysts and thickening of this structure, just like a sponge absorbs water.
RISK FACTORS
The main risk factors for the above changes to occur are:
- Duration of diabetes: the longer the duration of diabetes, the more likely these changes will be present when examining the back of the eye
- Poor diabetic control: the higher blood sugar levels are long-term, the more likely it is for DR to progress into more advanced stages
- Pregnancy: can sometimes lead to progression of DR
- Hypertension, hyperlipidaemia, smoking: all the above accelerate the damage affecting the vessels of the retina and can only lead to worsening of DR.
TREATMENTS
The best treatment is prevention! Regular ophthalmological check-ups are essential so that early changes are picked up and more effort is then put towards to a tight blood sugar control. Should intervention be required there are a number of treatments that George Morphis can perform where appropriate.
- Panretinal Laser Photocoagulation (PRP): Laser can be applied to the retina to make the defective vessels regress and prevent the worst complication of PDR, which is bleeding into the vitreous gel which may cause severe vision loss.
- Macular Laser: This is more gentle laser applied to the macula to stop the vessels from leaking fluid. It is aimed to stabilize the vision in the majority of cases or slightly make it better.
- Intravitreal injections: The last few years, the so called anti-VEGF injections have become available. They work by reducing the leakage of the defective vessels and accelerate the absorption of excess fluid which causes vision loss. It is like squeezing a sponge soaked with water!
- Vitrectomy: This refers to the surgical approach for treating proliferative diabetic eye disease. It involves removing the vitreous gel of the eye which most of the time is mixed with blood. Following this, endolaser is applied on the retina to make all defective vasculature regress.
SUMMARY
Every patient with diabetes should have regular eye check-ups by a retina specialist to determine whether there is damage in the back of the eye. Patients should also follow an appropriate diet and be compliant with all medicines they take.
In cases where sight threatening damage is found, George Morphis will discuss with you appropriate treatment. This can be retinal laser, injections or even surgery (vitrectomy) depending on circumstances.